As I got towards the end of my treatment, in early 2009, I was inching my way closer to freedom and returning to school. But, my plans were thrown out the window as the H1N1 influenza (also known as Swine Flu) pandemic took over the US (where I lived at the time). After discussion with my doctor, my parents and I decided that I should stay home and avoid attending school for a few more months. This was perhaps the most difficult time because I was finally physically feeling better, so I felt the limitations even more.
11 years later, all of the hype around social distancing feels strange because I’ve seen how cancer patients, survivors, and anyone living with an immuno-compromising condition, have been social distancing pros for years already. It’s just that social distancing wasn’t instagram-able until the rest of the world had to do it too. So, if you’re struggling with the idea of social distancing and how you’ll cope with the foreseeable future in isolation, reach out to someone with experience (Just not in-person!). I’m sure they’ll have lots of useful advice to share!
In case you don’t know anyone with this kind of expertise, or if you’re newly living with a socially-limiting illness yourself, I’ll share with you my top 5 pieces of advice for how to manage life at home, on your own.
- Have an accountability buddy or find ways to hold yourself accountable for your work. While I was on treatment, I was lucky to have a home/hospital tutoring program provided by my county in the US. This meant that they sent a teacher to my school to pick up my assignments from my school teachers, spend 6 hours per week in my home and go through new lessons with me. For the other 34 hours, I had to get through assignments on my own. But, expecting my teacher’s visit on the same days each week meant that I had someone holding me accountable. Alternatively, if you don’t have someone to hold you accountable, consider setting some deadlines for yourself.
- Make a schedule for yourself – including time for things you enjoy or other tasks that you need to do around your home. Days without structure can seem fun at first, but soon they become frustrating and can contribute to a sense of hopelessness/lack of accomplishment. On the other hand, too much work can burn you out. Your brain will take some time to acclimate to being on its own (it’s amazing how much harder it is to work when you’re not surrounded by other people working). You might also have distractions around you to navigate. Consider these things when making a schedule for yourself, and possibly consult your teachers or supervisors. Making a schedule will also help you protect your personal time so you can do some things you enjoy in your free time.
- Ensure you plan at least one achievable task/goal each day. When you’re stuck at home, it can be really helpful to get some sense of accomplishment each day, to remind you that you are making good use of your time. I always found it useful, as I started each day, to choose one achievable task that I knew I could and would get done that day. That way, whether fatigue limited my work hours or chemo-brain limited by working speed, I could still say I got something done.
- Pay attention to your feelings and talk about them – virtually with friends, or in person with people living with you. Being at home 24 hours per day, 7 days per week gets old. Really fast. You’ll find yourself having moments of loneliness, frustration, boredom, lack of focus, etc. Pick up the phone and call a friend or relative. Use your video call service of choice to connect with your workmates or classmates. You can be physically isolated but you don’t have to be socially isolated! Also, remember that distancing and isolation don’t last forever. Whether you have to make it through flu season, a pandemic, or 2.5 years of cancer treatment, remind yourself that you just have to keep moving forward.
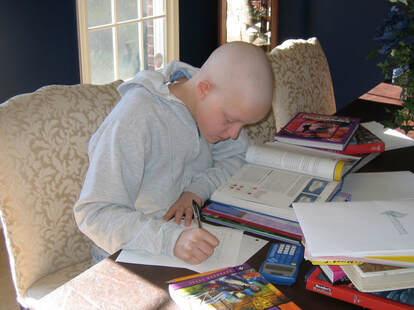
- Choose a single space in your home as your workspace. When I was sick, it was my parents’ dining room table. We extended it out as far as it would go, then I took over half of it. Pick a space with as much natural light as possible, and preferably with a window nearby – it’ll help you keep awake and focused. Try to separate your work space from your leisure space where possible – like I try to limit my use of my kitchen table to work and meal times.
Instead of letting this adversity become problematic, it’s a great time to consider how we can find new opportunities - opportunities for each of us to learn more about ourselves, spend more time with those we live with, learn new hobbies or skills, test out new ways of working and getting things done, or helping others who may be struggling. By social distancing, we may find better ways of getting and staying connected to one another. Most importantly, we won’t take for granted how lucky we are when we can get up in the morning and leave our homes to go to work or school.

 RSS Feed
RSS Feed