We conducted a narrative review to address this research gap. Overall, we found that evidence points to the importance of introducing palliative care teams earlier. Additionally, it is important to explore AYAs’ preferences around end-of-life issues in a repeated, consistent manner; this offers multiple ‘openings’ to these difficult conversations, and also allows for the fact that AYAs’ preferences can and do change over time as their medical and support needs change. Our review also highlighted that AYAs may have strong preferences on a range of issues such as being able to stay in their own home, being comfortable and free from pain, and expressing their wishes to loved ones.
We highlighted a number of best-practice recommendations to guide clinicians around the critical elements of when, who, what, and how end-of-life conversations may be best had with AYAs. These included:
- When: Introduce palliative care team members earlier during treatment to facilitate opening conversations to end-of-life concepts prior to disease/symptom-related ‘crises’ or the end of active (curative) treatment.
- Who: Ensure the wider multidisciplinary team is confident and adequately skilled to support end-of-life conversations with AYAs.
- What: Tailor the content of end-of-life conversations to the individual patient, and the unique context of the particular time point the conversation is being introduced.
- How: Use structured advance-care planning tools to scaffold conversations, and as a mechanism to facilitate communication between AYA patients, their families, and members of the multidisciplinary care team.
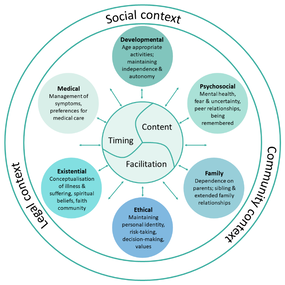
Numerous gaps in the evidence base remain. For example, there is a lack of data to guide practice when disagreement between AYAs’ and their parents’ preferences exists. However, based on our research synthesis, we proposed a new model (below) to support clinicians and researchers to better understand how individual, familial, and socio-cultural factors impact end-of-life communication with AYAs in clinical settings. We hope this model will continue to spark new research questions and support clinical advocacy for AYAs with cancer and their families facing end-of-life.
Figure 1: Model of the developmental context for end-of-life communication with AYA cancer patients.
 RSS Feed
RSS Feed