Background
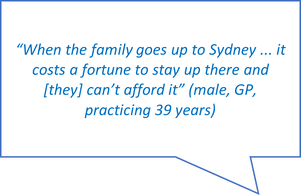
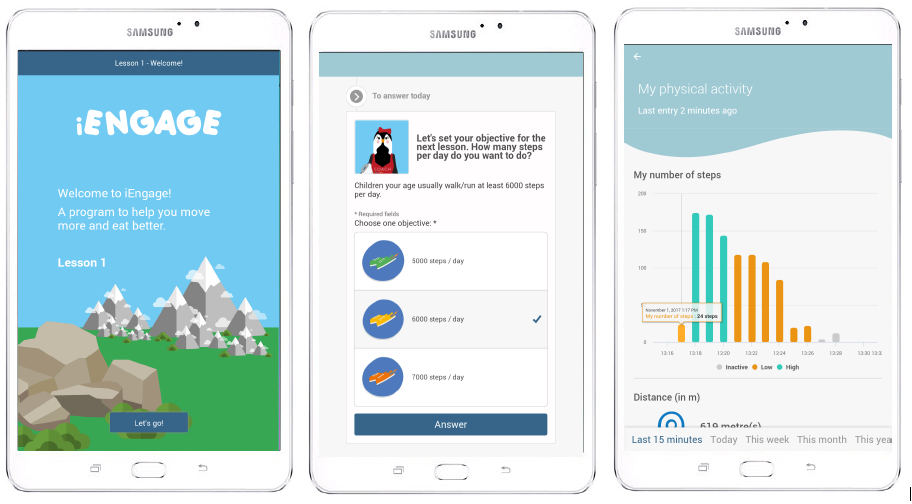
Health behaviour education is very important, though often lacking in childhood cancer treatment. Health behaviour education includes, but is not limited to, physical activity and healthy eating. Physical activity and healthy eating are important habits for childhood cancer survivors (survivors) to have so they can live a healthy life after cancer. It is important to cater to survivors wants and needs when teaching survivors about physical activity and healthy eating. Therefore, we spoke to survivors, their parents and health professionals to learn exactly what they would like to see in an online physical activity program.
Our study
We spoke to 9 survivors, 13 parents and 18 health professionals. Before the discussions, everyone completed a survey that provided a range of online health features. The survey asked everyone to rate the importance of these features for survivors. One example of a feature was, “Providing physical activities that involve family.” The most and least important features were discussed.
Our findings
Most important online health features:
- Physical activity and healthy eating education
- Setting and viewing goal achievements
- Physical activities that involve family and friends
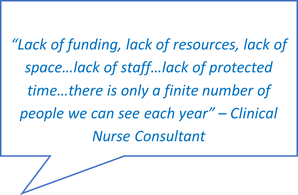
- Health professional support
Least important online health features:
- Quizzes to deliver education
- Viewing other participants’ physical activity levels
- Paper as a mode of education delivery
Design Tips:
- Videos to deliver education
- Age appropriate
- Concise
When do participants want online physical activity education:
- As soon as possible
Future steps
We learnt what health behaviour education that survivors would benefit from and how to deliver it. These findings helped our research team develop the new online physical activity program, Making Moves. Making Moves teaches survivors age-appropriate healthy behaviours. We hope Making Moves provides important information to living a safe and physically active life after cancer.
Making Moves is in the research phase and is open for participation by young people affected by cancer. You can join the study if you:
- Are currently aged 8-21 years.
- Were diagnosed with cancer under 18 years.
- Have completed cancer treatment at least six months ago OR have been on maintenance therapy for at least six months.
Please click here to learn more and register you or your child’s interest in participating in the Making Moves program.
Click here to read the full article.




 RSS Feed
RSS Feed