Managing health after cancer: Survivorship care services are available for survivors to effectively manage these long-term health problems. Research shows that survivors who are engaged in long-term follow-up care have better physical and psychosocial outcomes in childhood cancer survivors. Yet many survivors don’t receive follow-up care leading to missed opportunities for surveillance and early intervention, including screening and healthy lifestyle education). Poor engagement in follow-up care indicates that current models of survivorship care need improvement.
New models of survivorship care: The success of any model of survivorship care requires aligning with key stakeholders’ needs and preferences, including survivors and healthcare professionals. In our recent survey study, we aimed to learn about survivors’ engagement in survivorship care, barriers to accessing follow-up care, their satisfaction with care, and preferences for receiving future care. To achieve this, we surveyed 633 participants in total; including 187 parents of young survivors, 251 adolescent and young adult survivors (AYAs) and 195 older survivors from 11 hospitals across Australia and New Zealand. Of these survey participants, 151 also completed an optional telephone interview to help us learn more in-depth about their experiences and preferences.
Satisfaction with care: Worryingly, up to 70% of long-term survivors were not engaged in follow-up care. Engagement in follow-up care was significantly lower in older survivors of childhood cancer, yet the number of cancer-related health conditions they reported were much higher. Survivors who reported receiving follow-up care were more satisfied with their care than those not receiving cancer-related care.
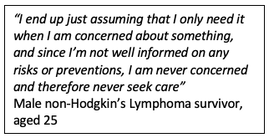
Barriers to survivorship care: Survivors reported many barriers to accessing survivorship care, most commonly i) 67% had a poor understanding about the need for, or availability of, follow-up care, ii) 65% experienced logistical barriers such as not having appointment reminders, and iii) 57% reported that the costs associated with attending follow-up clinic prevented them from going, including the cost of travel or taking time off work. Another important barrier was the emotional challenge of returning to the hospital where they, or their child, was treated as it brought back painful memories for them. Further analysis showed that survivors reported a great number of total barriers to accessing care if they were older, a longer time from diagnosis, and lived further away major cities. This suggests that older and more geographically isolated patients need more support to access survivorship care.
Preferences for future care: even though survivors reported many difficulties to accessing survivorship clinics, most preferred to receive specialised follow-up care delivered through oncologists, survivorship nurses and multi-disciplinary teams. Fewer survivors preferred their survivorship care to be delivered through community based follow-up, specifically general practitioner’s (GP). Survivors seemed to have low confidence in their GP’s ability to offer survivorship care, possibly due to their GP’s lack of involvement during their cancer treatment, and the strong connection many establish with primary treating oncology team. This represents a key challenge for healthcare systems, as survivorship clinics are under resourced to manage the growing population of long-term survivors of childhood cancer.
Importance of these findings: Our findings offer insight into how best we can deliver survivorship care, to cater to survivors’ and parents’ preferences and to ensure that the survivorship needs of this vulnerable population are adequately met. Given that many high-risk survivors are disengaged from cancer-related care, identifying patient preferences can be used to re-engage survivors who should be receiving cancer-related follow-up. Future research should evaluate healthcare professional preferences to ensure system- and physician-reported barriers are also considered in developing an optimal model of care for survivors of childhood cancer. Aligning survivors’, physicians’, and system needs will remain a challenge in developing a preferred and yet sustainable model of care.
This blog post was written by Dr Christina Signorelli and Mr Joe Alchin. The original manuscript has been published in BMJ Supportive & Palliative Care Journal at: https://spcare.bmj.com/content/early/2019/11/11/bmjspcare-2019-002001
 RSS Feed
RSS Feed