Medical procedures in children are common, and can cause anxiety, pain and distress in children and in their parents or carers. Pharmacological (i.e. medication) and non-pharmacological (i.e. distraction) approaches are often used to minimise procedural pain and anxiety. Although effective, pharmacological approaches often cause negative side-effects. On the other hand, non-pharmacological are effective approaches which can include therapy play to promote education and coping, or distracting children from their pain or anxiety associated with medical procedures.
Screen-based technologies are increasingly common non-pharmacological resources being used to improve procedural pain and anxiety in paediatric care. They can involve passively watching a video or actively playing a computer game (i.e., interactive video games).
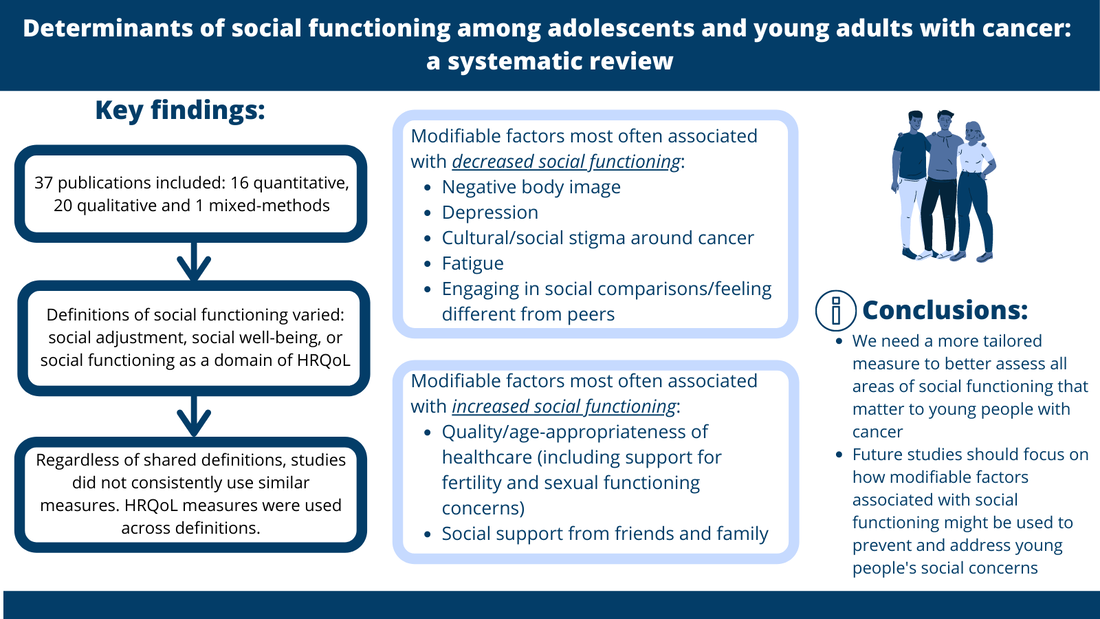
Though research has shown that screen-based technologies can reduce procedural pain and anxiety, we still do not know much about the effectiveness of screen-based technologies depending on the extent to which the user engages with such technologies. We might expect that active engagement with technology may result in lowered pain perception due to greater immersion with the technology. It is also unclear if interventions that educate patients about their upcoming procedure (i.e., preparatory interventions) are more effective than interventions that simply aim to reduce pain and anxiety through distraction alone. We therefore reviewed the available literature covering a 20-year period to understand the strength and nature of existing evidence.

We systematically identified, located
and accessed experimental studies that examined the effect of video games interventions on procedural pain and anxiety among children (aged 0–18
years). Through our systematic search
of the literature, we identified 36
relevant studies representing 3406
young patients. The evidence suggests that children who used interactive video games reported less pain and anxiety compared to children who used other types of interventions (e.g. clown therapy). The studies also showed that playing interactive video games were more effective at reducing children’s procedural anxiety compared to passive games. The evidence also showed that carers of children who played interactive video games reported lower anxiety than carers of children who used other interventions.
Our review supports the use of interactive video games to reduce procedural pain and anxiety in children, and their carers. Although we did not observe any substantial benefits of preparatory video games over distraction-based ones. It remains unclear though about the best timing and setting to implement interactive video games to achieve the maximum benefit on patient outcomes, for example if repeated exposure may further reduce pain and anxiety in children undergoing medical procedures.
This article was published in the British Journal of Anaesthesia. The full paper can be found here.
This post was written by Dr Christina Signorelli and Mr Sylvester Okeke.


 RSS Feed
RSS Feed